Hi friends,
Sorry I’ve been AWOL for a few months – every time I’ve sat down to write something, I’ve felt like I have nothing to say (despite an ever-growing list of blog ideas in my phone). I don’t really know what I want this blog to be other than honest and authentic, and I don’t think I can publish on a set schedule while being authentic. That being said, I just got out of an appointment and I felt an overwhelming desire to just get some of my thoughts and feelings out.
The Appointment
A few months ago (like, 5ish), my husband and I agreed we finally felt ready to grow our family and try for a 2nd baby. At this point, I did the ‘responsible’ thing and let my doctor know that we were about to start trying to conceive, and asked if I should know or do anything special before we embarked in earnest.
While I had only been seeing this doctor for a few months at this point, we had discussed my weight before and I had felt some sense of confidence that he was going to be a HAES (health at every size) practitioner I could feel safe with. This is why I was stunned when he suggested that one of the best ways I could prepare for a healthy pregnancy was to lose weight.
Before I get too far with this story, I just want you to know that it is possible, and downright common, for a fat woman to have a healthy pregnancy. I did it before, and I have many girlfriends who have done it too. I know this stuff – I have been consuming Intuitive Eating and Fat Liberation content for over a year. I said nothing to my doctor when he suggested I try to lose weight, and even less when he referred me to a weight management clinic. I came home taken-aback and dazed, and didn’t really process those feelings until the day of my appointment.
On the day of that appointment I woke up acutely aware of how nervous and frankly afraid of opening this door I was. I had spent over a year working hard to deconstruct the diet culture I had been consuming my entire life. Working hard to build up confidence in the fact that my value in the world didn’t go down when the number on the scales went up. I had been working with a therapist to understand my own relationship with my body, and developing boundaries to protect it. Yet here I was – about to discuss intentional weight loss plans with a weight management clinic.
To allay these fears, I kept telling myself that I liked and trusted my Doctor, and that he wouldn’t refer me to something harmful. I also confided in my best friend, who reassured me that I know how to advocate for myself. So I went into that first meeting nervous, but hopeful. Maybe the clinic would just talk to me about my history, and we could discuss ways for me to focus on health and movement without weight loss as the standard of success.
The appointment began well, the Doctor I spoke with asked me about my history, why I was being referred now, and what I hoped to get out of this experience. I explained my history, my recent journey with Intuitive Eating, and how I didn’t want to focus on weight loss or restriction, but that I was willing to work on overall health goals by exploring nutrition variety and adding more movement to my life. She looked at my recent bloodwork, which she said she had no concerns about, and said she ‘loved’ that I had already begun to break down diet culture because the evidence is clear that diets do not improve health or result in long term weight loss.
I was so excited about how the rest of this meeting might go. Maybe this would be the motivation I needed to find movement I love and make it a regular part of my life. Then I was hit with the ol’ bait and switch. She went from agreeing with all my Intuitive Eating values, to asking if I would be opposed to taking prescriptions that could help me lose weight.

I froze. I didn’t know what to say or how to react. I didn’t feel like I could outright say no to her; she was the doctor and maybe she knew best. The response I mustered up was “I guess it would depend on the medication and any potential side effects”. Not a ‘no’, not a ‘Hell No’, not a ‘FUCK NO’ – which is what that question deserved. She had just finished telling me that my bloodwork was good. No high cholesterol, no elevated blood sugars, no medical reason to medicate me, other than to get me into a smaller body.
At the end of the appointment, she recommended I proceed with a consultation about nutrition, but in the meantime I should start tracking what I eat. So I started to track what I was eating. All my old habits came back – worrying about eating enough raw vegetables, concerned about how my ‘splurge’ consumption of a cinnamon bun, or a fun pub-food night with friends would change what this team of strangers thought of me.
Now we arrive at today. I have just finished that follow up appointment about ‘nutrition’. I don’t know why what I’m about to share with you surprised and deeply upset me, but even after a year of deconstructing diet culture – it still did.
Instead of consulting me on nutrition, she informed me of the programs available through this weight management clinic. The first of which costs almost $800. This would include regular check-ins with a Registered Dietitian, a few appointments with an exercise therapist, and regular check ups with the original Doctor I had spoken with. Then she reviewed the ‘Free’ program with me (free being the services covered by AHS), this program didn’t offer meetings with registered Dietitians, but “health consultants” like herself, and no meetings with the exercise therapist. She stopped and asked me which level of program I would be interested in.
I must have finally found that ability to advocate that my best friend believed in, or maybe I finally heard enough BS to snap me out of my stupor – but my response was something along the lines of “I’m sorry, I thought this was already going to be an appointment about my nutrition, with a Dietitian or Nutritionist? Not a sales pitch for a weight loss program that costs me money. I thought I was receiving health care through AHS?”. She temporarily wavered, and then reassured me that the ‘free program’ was available, and reviewed what was included in that. I followed up by asking ‘OK, what exactly is a Health Consultant? If you’re not a Dietitian or a Nutritionist or a Doctor, if you don’t mind me asking, what exactly are you?”
I need you to know that I was taking notes in this meeting, because I take my health seriously, so what follows are direct quotes from how she described herself:
“A health consultant is essentially a nutritionist – just not a registered dietitian. Like, I’m not a member of any professional body, but I have essentially the same education. And I also can do exercise stuff.”

She used “essentially” a few more times, so I stopped taking notes and just wrote down “What the fuck?” … We never reviewed my food log.
Diet culture is so insidious. It pretends to be worried about your welfare, so it is often perpetuated by well meaning people. I’m sure this lady thought she was really helping me. I’m sure my doctor believes he is recommending what is best for me. But I left that meeting feeling stupid, afraid, angry, and had received zero scientifically sound advice in 2 different meetings with ‘experts’.
Still Trying
So where does that leave me and my journey to becoming a mother of 2? Where I always was. I am still trying. Every month that I get my period is another month of heartbreak. I think that’s part of why I haven’t written in a long time. Subconsciously I was hoping that my next posts could chronicle my plus sized pregnancy. Instead, I’m here writing about how my desire to have a positive pregnancy led me down a months-long path of getting duped into another diet culture attack.
I KNOW I can have a healthy pregnancy. Besides severe HG, wherein I actually lost weight, I had a VERY healthy pregnancy. My son developed ‘normally’, I never had any pregnancy related complications (like Gestational Diabetes, Gestational Hypertension, Pre-eclampsia, etc.) and I was able to have a relatively uneventful vaginal delivery. Even if I had any of these complications, I know that they can and do occur in thin-bodied pregnancies too.

Furthermore, I know that my pre-pregnancy self is relatively healthy. I have no current diagnoses to treat, let alone any conditions associated with obesity. So why did asking my doctor about a healthy pregnancy lead down this road? Why didn’t he just ensure I was taking prenatal vitamins and tell me to stop drinking? Why didn’t he recommend that I start and/or continue to move my body? Or remind me that I should stop taking Advil? Aren’t these the messages he would have delivered to a woman trying to conceive in a smaller body?
SIDE NOTE: One of the most common ailments that hinders our ability to conceive is PCOS. I am SO sorry if you live with PCOS, it sounds horrible, and it’s not fair. Most doctors will tell you that losing weight is your first (and only) option – they say it not only helps improve your PCOS, but will enable you to get pregnant. This is all kinds of misleading and unfair. PCOS exists in thin people, and as @DrHeatherIrobundaMD points out in the caption for this post, even the American College of Obstetricians and Gynecologists classifies weight loss “as a Level B recommendation/conclusion (meaning that it’s based on limited or inconsistent evidence).”
Weight Stigma is more harmful than excess weight itself
So here’s the bitch of a plot twist – Being fat is not going to prevent me from having a healthy pregnancy, but fat discrimination in medicine will. In one recent review, researchers found that:
I included that quote as a summary, but really this whole paper is worth reading. If you have the time and inclination, I highly recommend. In fact, one of the researchers on that paper, Angela Incollingo Rodriguez, has dedicated the last few years of her career, and her research lab, to further understanding the impact of weight stigma on women, particularly during pregnancy and the post-partum period.
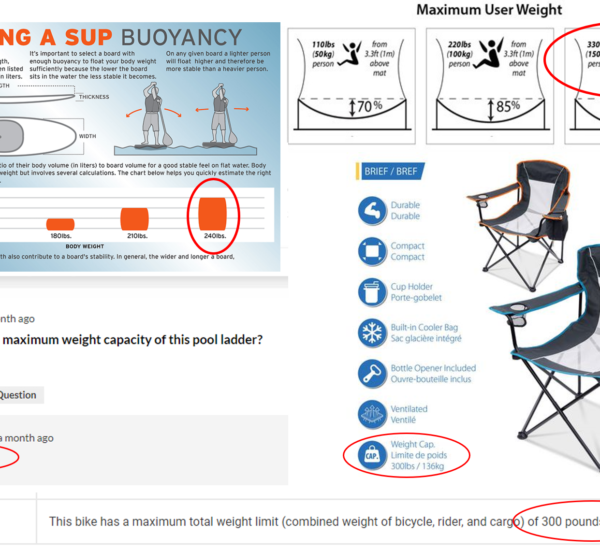
Weight stigma is a common enough reality for anyone in a larger body, but it increases as soon as people in larger bodies try to procreate. We are told we need to lose weight to have healthy pregnancies (patently untrue), we are prevented from accessing fertility treatments, told it’s unsafe for us to use alternative avenues of care, like midwives, and are referred to high-risk clinics. Beyond that, there’s the ‘normal’ weight discrimination we receive as fat women, which includes increased wage penalties, implicit and explicit weight bias expressed by medical students, less time discussing our health during primary care visits, and shortened life expectancy.
One meta-analysis published in 2011 found that:

All of these factors result in a system of self-fulfilling prophecy. Women who can’t access good fertility treatment conceive less often. Women who can’t access midwives or alternate avenues of care will have pregnancies and deliveries with more medical intervention. We are often encouraged to consider getting induced or having scheduled C-sections, which reinforces the belief that we are unable to trust our bodies to safely deliver our babies.
I also know that a lot of this prejudice and discrimination is mitigated by my status as a white woman with a lot of privilege. Racialized minority groups experience additional workplace and medical discrimination that compounds and contributes to weight stigma.
Now what?
So what do we do? I don’t know. There is no silver bullet. Ideally we could all find safe, HAES care, but that’s not the reality of the situation, especially during COVID when healthcare resources are stretched thin. I know what I’m going to do. I’m going to continue to advocate for myself when I am able. I will continue to arm myself with evidence that I do not need to lose weight to have a healthy pregnancy, and try to challenge my medical team when they insist I need to use a high-risk OBGYN team rather than enlisting a midwife. I will surround myself with people and resources that reaffirm rather than cast doubt on my ability to get pregnant and carry a healthy baby to term without taking prescriptions with unnecessary side effects to reduce my body size.
For more information on fat fertility I HIGHLY recommend the account @fatpositivefertility on Instagram run by Nicola Salmon, an incredible resource for people like us! I also recommend @PlusSizePregnancy for information on how to advocate for yourself once you are pregnant. I’ll keep you posted, and hopefully I will have good news soon, but if I don’t I’ll remind myself that it’s not my fault.
Citations
Hill, B., & Incollingo Rodriguez, A. C. (2020). Weight stigma across the preconception, pregnancy, and postpartum periods: A narrative review and conceptual model. Seminars in Reproductive Medicine, 38(06), 414–422. https://doi.org/10.1055/s-0041-1723775
Irobunda, H. (2021, September 8). Weight is not the only thing to consider when talking about PCOS. Instagram. Retrieved October 21, 2021, from https://www.instagram.com/p/CTkYRJlM12w/?utm_source=ig_web_copy_link.
Krueger, P. M., & Reither, E. N. (2015). Mind the gap: Race/ethnic and socioeconomic disparities in obesity. Current Diabetes Reports, 15(11). https://doi.org/10.1007/s11892-015-0666-6
Maranto, C. L., & Stenoien, A. F. (2000). Weight Discrimination: A Multidisciplinary Analysis. Employee Responsibilities and Rights Journal, 12(1), 9–24. https://doi.org/10.1023/a:1007712500496
Mulherin, K., Miller, Y. D., Barlow, F. K., Diedrichs, P. C., & Thompson, R. (2013). Weight stigma in maternity care: Women’s experiences and care providers’ attitudes. BMC Pregnancy and Childbirth, 13(1). https://doi.org/10.1186/1471-2393-13-19
Phelan, S. M., Dovidio, J. F., Puhl, R. M., Burgess, D. J., Nelson, D. B., Yeazel, M. W., Hardeman, R., Perry, S., & Ryn, M. (2014). Implicit and explicit weight bias in a national sample of 4,732 medical students: The Medical Student Changes Study. Obesity, 22(4), 1201–1208. https://doi.org/10.1002/oby.20687
Puhl, R. M., & Heuer, C. A. (2010). Obesity stigma: Important considerations for public health. American Journal of Public Health, 100(6), 1019–1028. https://doi.org/10.2105/ajph.2009.159491
Sutin, A. R., Stephan, Y., & Terracciano, A. (2015). Weight discrimination and risk of mortality. Psychological Science, 26(11), 1803–1811. https://doi.org/10.1177/0956797615601103
Comments